Uncategorized
Coverage Mandated for Rapid At-Home COVID-19 Tests
By: Emily H. Lineweaver
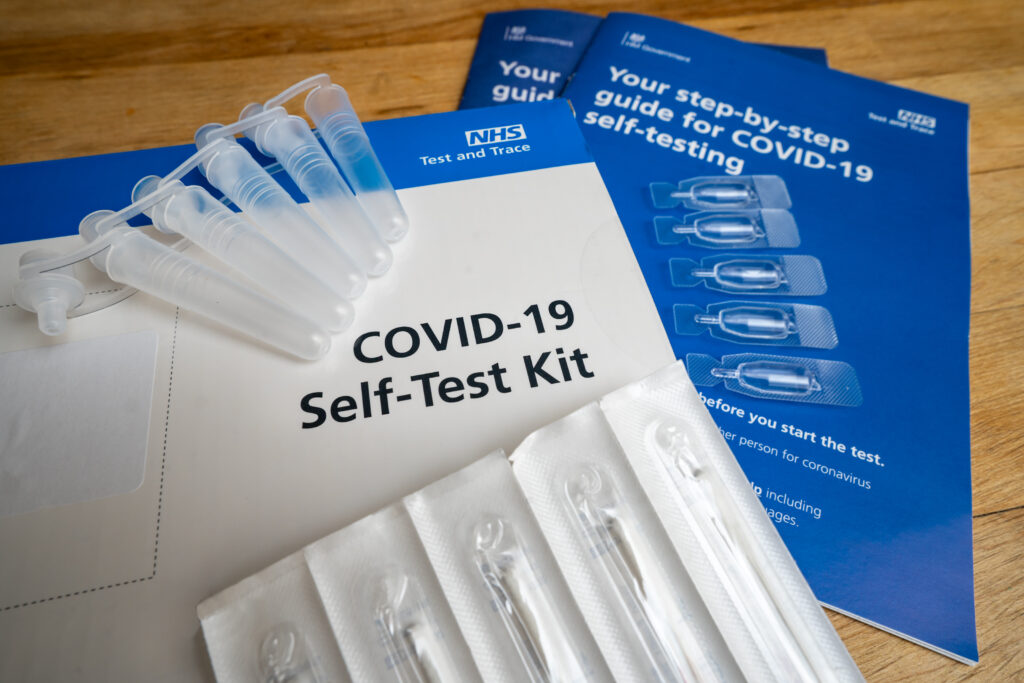
On January 10, 2022, the Biden-Harris Administration, through the Centers for Medicare & Medicaid Services, issued a new policy mandating private insurance companies and group health plans cover the cost of at-home, rapid COVID-19 test kits beginning January 15, 2022. The program allows insurers to set up networks of preferred suppliers in order to make individual tests available with no up-front costs. However, insurers will still be required to reimburse covered individuals in a plan at a rate of up to $12 per individual test if they purchase outside of the preferred network. The policy also requires coverage of up to 8 individual tests per person enrolled in the plan per month.
In a statement regarding the new policy, the Department of Health and Human Services Secretary Xavier Becerra said, “By requiring private health plans to cover people’s at-home tests, we are further expanding Americans’ ability to get tests for free when they need them.”
